Infant eczema: causes and remedies
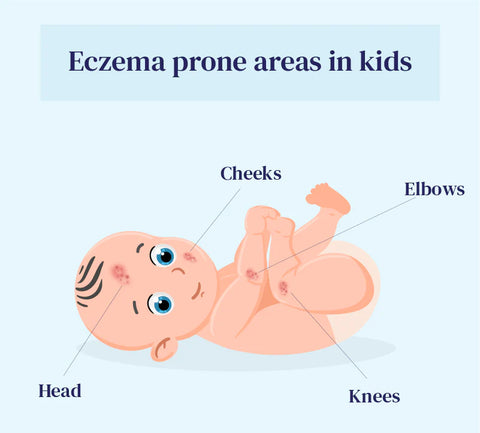
Baby eczema, also known as infantile or atopic dermatitis, is a common skin condition affecting infants and young children. It is characterized by red, dry, itchy patches of skin that may become inflamed, scaly, or even cracked. Baby eczema can appear anywhere on the body but is often found on the face, scalp, cheeks, and in the folds of the skin, such as behind the knees and the creases of the elbows. According to the National Eczema Association, baby eczema affects about 9.6 million children and about 16.5 million adults in the US.
The exact cause of baby eczema is not fully understood, but like in adults, it is believed to involve a combination of genetic, environmental, and immune system factors. Babies with a family history of eczema, asthma, or allergies may be more likely to develop baby eczema.
Triggers for baby eczema can include irritants like harsh soaps or detergents, allergens like pet dander or certain foods, dry skin, changes in temperature or humidity, and stress. Scratching or rubbing the affected areas can further irritate the skin and worsen symptoms.
Treatment typically involves gentle skincare practices such as using mild, fragrance-free cleansers and moisturizers, avoiding irritants and allergens, and keeping the baby's skin well-hydrated.
While baby eczema can be uncomfortable and distressing for both the infant and their parents or caregivers, most cases improve with proper skin care and treatment, and many children outgrow the condition by early childhood.
What Causes Eczema in Babies?

The exact cause of baby eczema, like eczema in older children and adults, is not fully understood. However, several factors may contribute to its development:
- Food allergies: Some babies may develop eczema due to food allergies or sensitivities. Common food allergens associated with eczema include cow's milk, eggs, peanuts, soy, wheat, and fish.
- Genetics: Family history significantly affects the likelihood of a baby developing eczema. Children with parents or siblings who have eczema, asthma, or allergies are more likely to develop eczema themselves, suggesting a genetic predisposition.
- Immune system dysfunction: Eczema is considered to be related to an overactive or dysfunctional immune system response. The immune system may react abnormally to certain triggers in individuals with eczema, leading to skin inflammation and irritation.
- Skin barrier dysfunction: Babies with eczema often have a compromised skin barrier, which allows moisture to escape more easily and makes the skin more susceptible to irritants and allergens. Factors contributing to a weakened skin barrier include genetic, environmental, and disruptions in the skin's natural lipid barrier.
- Environmental factors: Exposure to certain environmental factors can trigger or exacerbate eczema symptoms in babies. These may include irritants such as harsh soaps, detergents, fabrics, chemicals, and allergens like pet dander, pollen, dust mites, and certain foods.
- Dry skin: Dry skin is a common trigger for eczema flare-ups in babies. Low humidity levels, cold weather, excessive bathing, and harsh skincare products can all contribute to dryness and exacerbate eczema symptoms.
It's important to note that eczema triggers can vary from one baby to another, and what triggers eczema flare-ups in one child may not affect another child similarly. Identifying and avoiding triggers, maintaining proper skincare, and seeking medical treatment when necessary can help manage and alleviate eczema symptoms in babies.
How can parents recognize eczema in babies?
Parents can recognize eczema in babies by observing certain signs and symptoms on their baby's skin. Here are some common indicators to look out for:
- Red or inflamed patches: Eczema often appears as red or inflamed patches of skin on the baby's face, scalp, cheeks, arms, legs, and in the folds of the skin (such as behind the knees and in the creases of the elbows).
- Dry, scaly skin: Affected areas of the skin may be dry, rough, or scaly to the touch. The skin may also feel rough or coarse, especially during flare-ups.
- Itching and discomfort: Babies with eczema may show itching, rubbing, or scratching the affected areas. They may also appear restless or irritable due to discomfort and itching.
- Rash or bumps: Eczema can cause the development of small bumps, blisters, or raised patches of skin, which may ooze or crust over if scratched excessively.
- Thickened or leathery skin: Prolonged eczema can lead to thickening or hardening of the skin, especially in areas that are scratched frequently.
- Worsening symptoms with triggers: Eczema symptoms may worsen or flare up in response to certain triggers, such as exposure to irritants (e.g., harsh soaps, detergents) or allergens (e.g., pet dander, pollen).
- Poor sleep patterns: Babies with eczema may experience disrupted sleep patterns due to itching and discomfort, leading to irritability and fatigue.
If parents notice any of these signs or symptoms on their baby's skin, consulting with a healthcare professional, such as a pediatrician or dermatologist, is essential. An accurate diagnosis and appropriate treatment plan for eczema can help alleviate discomfort and prevent further complications.
Types of Children's Eczema
Various types of eczema can manifest in children, each with distinct characteristics. Some of the most common types of eczema in children include:
- Atopic dermatitis: This is children's most common form of eczema. It often appears as red, itchy patches on the skin, particularly on the face, scalp, arms, and legs. Children with atopic dermatitis often have a family history of eczema, asthma, or allergies.
- Contact dermatitis: This occurs when the skin comes into direct contact with an irritant or allergen, leading to inflammation and redness. Common triggers include certain soaps, detergents, fabrics, plants, and metals (such as nickel). Symptoms typically appear on the area of skin that has been in contact with the irritant or allergen.
- Seborrheic dermatitis: Also known as cradle cap in infants, it often affects the scalp and appears greasy, yellowish scales or crusts. It can also occur in other areas with oil glands, such as the eyebrows, ears, and diaper area. Seborrheic dermatitis is not typically itchy but can be persistent.
- Nummular eczema: This form of eczema is characterized by round, coin-shaped patches of red, inflamed skin that may ooze or crust over. It often occurs on the arms and legs and can be triggered by dry skin, irritants, or allergens.
- Dyshidrotic eczema: This typically affects the hands and feet, causing small blisters on the palms, fingers, soles, or toes. The blisters may be intensely itchy and can lead to redness, swelling, and peeling of the skin.
- Allergic contact dermatitis: Allergic contact dermatitis occurs when the skin comes into contact with an allergen, triggering an immune response and causing redness, itching, and inflammation. Common allergens include certain metals (such as nickel), fragrances, preservatives, and topical medications.
- Asteatotic eczema: Also known as eczema craquelé, typically affects older children and adolescents. It is characterized by dry, cracked, and fissured skin, often appearing on the lower legs. Asteatotic eczema is commonly exacerbated by low humidity and excessive bathing or washing.
These are just a few examples of the different types of eczema that can affect children. Proper diagnosis and treatment by a healthcare professional are essential for managing eczema symptoms effectively.
What is the difference between acne and baby eczema?
This is a common question that is often asked. Baby eczema and baby acne are two common skin conditions affecting infants but have different causes, characteristics, and treatments.
- Baby Eczema (Atopic Dermatitis):
- Cause: Baby eczema is a chronic inflammatory skin condition often linked to genetic factors, allergies, and immune system dysfunction.
- Characteristics: Baby eczema typically appears as red, dry, itchy patches of skin that may be rough, scaly, or inflamed. It commonly affects the face (especially the cheeks and forehead), scalp, arms, and legs. Eczema patches may also ooze, crust over, or become thickened with prolonged scratching.
- Triggers: Eczema flare-ups can be triggered by irritants (e.g., soaps, detergents), allergens (e.g., food, pet dander, pollen), dry skin, changes in temperature or humidity, and stress.
- Treatment: Treatment for baby eczema typically involves gentle skincare practices, moisturizers, adjusting food intake, avoidance of triggers, and, in some cases, topical corticosteroids or other medications to help control inflammation and itching.
- Baby Acne (Neonatal Acne or Infantile Acne):
- Cause: Baby acne is a common, temporary skin condition due to the hormonal changes newborns experience shortly after birth. These hormonal changes can stimulate the baby's oil glands, leading to the development of acne.
- Characteristics: Baby acne usually appears as small red or white bumps on the baby's face, particularly on the cheeks, nose, and forehead. The bumps may resemble pimples or tiny whiteheads and are typically not itchy or painful.
- Duration: Baby acne usually appears within the first few weeks to months of life and tends to resolve on its own without treatment by the time the baby is a few months old.
- Treatment: In most cases, baby acne does not require treatment and will clear up independently over time. Parents should avoid applying harsh skincare products to the baby's skin and gently cleanse the affected areas with water and mild baby soap.
How is baby eczema treated?
Baby eczema is typically managed through a combination of skincare practices, lifestyle adjustments, and, in some cases, medical treatment. Here are some common approaches to treating baby eczema:
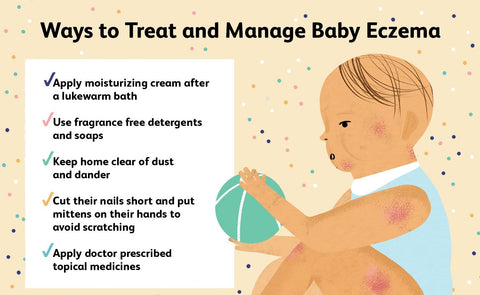
- Gentle skincare: Use mild, fragrance-free cleansers and moisturizers specifically formulated for sensitive skin. Avoid products containing harsh chemicals, perfumes, or dyes that may irritate the baby's skin.
- Keep the skin hydrated: Apply moisturizer to the baby's skin frequently, especially after bathing, to help lock in moisture and prevent dryness. Thick, ointment-based moisturizers are often more effective than lotions or creams for babies with eczema.
- Avoid triggers: Identify triggers that exacerbate eczema symptoms, such as certain fabrics, detergents, soaps, pet dander, pollen, and certain foods (if food allergies are suspected). Keep the baby's environment clean and free of dust and other allergens.
- Bathe in lukewarm water: Using mild, non-drying cleansers, bathe the baby in lukewarm (not hot) water. Avoid scrubbing or rubbing the skin harshly, and gently pat the skin dry afterward.
- Manage itching: Trim the baby's nails short to prevent scratching, and use soft cotton mittens or clothing to cover the hands during sleep if necessary. Keep the baby's bedroom cool and use lightweight, breathable clothing to prevent overheating.
- Medical interventions: A healthcare professional may prescribe oral antihistamines or oral corticosteroids to help control itching and inflammation. In severe or persistent cases of eczema, other treatments such as phototherapy (light therapy) or immunosuppressant medications may be recommended.
It's important for parents to work closely with a healthcare provider to develop a comprehensive treatment plan tailored to the baby's individual needs.
Hypoallergenic Formula For Babies with Milk Allergies
As highlighted earlier, understanding and avoiding triggers is key to effectively managing your baby's eczema. While milk allergies are not common among children, approximately 2-3% of babies have this condition, with eczema often as a common symptom of Cow's Milk Protein Allergy.
For babies allergic to milk protein, healthcare providers often suggest hypoallergenic formula. This proactive approach helps mitigate potential allergic reactions and supports your baby's overall health. If you suspect milk is a trigger for your baby's eczema flare-ups, it's crucial to seek medical guidance for an accurate diagnosis.
Hypoallergenic formula is specially tailored for babies who may be at risk for milk protein allergies. Despite being derived from cow's milk, this formula undergoes hydrolysis, breaking down the allergy-causing protein.
Through hydrolysis, the protein is fragmented into smaller compounds, easing digestion for infants. Because of this, the formula is less likely to trigger a potential allergic reaction when ingested.
Various types of hypoallergenic formulas exist, including extensively hydrolyzed, partially hydrolyzed, and amino acid-based varieties. In partially hydrolyzed formulas, milk proteins are only partially broken down to make them more easily digestible for the babies.
However, due to the partial breakdown, these formulas may heighten the likelihood of allergic responses. Conversely, extensively hydrolyzed formulas feature proteins completely broken down into minute compounds, thus minimizing the risk of allergic reactions.
Even with extensively hydrolyzed formulas, babies with cow milk allergies may still experience reactions. Therefore, this formula type isn't advisable for babies diagnosed with a cow's milk allergy.
EU-made Hypoallergenic Formulas

A wide range of hypoallergenic formulas are available on the market today. We carry EU-made HA formulas, and two of the leading brands in this category are HiPP and BebeM. HiPP, a renowned German formula manufacturer, boasts decades of expertise in crafting organic baby food products.
The Bebe-MT dairy-free vegan formula range is created with a unique 100% organic rice protein hydrolysate base. Bébé M has been certified organic by ECOCERT since 2013 and by AB France for its approach in selecting ingredients, formulation, and manufacturing.
What Makes HiPP HA Special?
HiPP Hydrolyzed Baby formula is designed for babies with a history of allergies or at a high risk of developing allergies. The HiPP Hypoallergenic formula comes in three stages, each tailored to meet the evolving nutritional needs of growing babies. Let's go a little deeper and explore the differences between HiPP Hypoallergenic Stage Pre, HiPP Hydrolyzed Stage 1, and HiPP Hydrolyzed Stage 2.
HiPP Hydrolyzed Stage Pre

It is designed for (premature) babies and infants up to 6 months of age. It is made from hydrolyzed protein, broken down into smaller pieces, making it easier for the baby's digestive system to process. This formula is an excellent choice for infants at a higher risk for allergies and intolerances, as hydrolyzed protein is less likely to cause an allergic reaction.
HiPP German HA Stage 1 HiPP Dutch HA Stage 1


This HA Formula is appropriate for infants from birth to 6 months of age. This formula is made from cow's milk protein that has been hydrolyzed, making it suitable for infants sensitive to allergens. Stage 1 also includes all the essential vitamins, minerals, and nutrients your baby needs to grow and develop.
HiPP German HA Stage 2 HiPP Dutch HA Stage 2


This HA Formula is designed for babies who are six months and older. Like breast milk, HiPP HA Combiotic Stage 2 features lactose as the primary source of carbohydrates and a blend of organic vegetable oils and essential vitamins and minerals. It also contains some starch to give the formula a thicker and creamier consistency since hydrolysis would otherwise produce a very thin product.
Good to know: Both formulas are very similar, with the added benefit of slightly higher protein amounts for the Dutch version (1.8g per 100ml) compared to the German version (1.3g per 100ml) to support the baby's growth and development. Furthermore, the German version comes in a 600-gr box, and the Dutch version comes in a stackable and easy-to-close 800-gr tin container.
What makes BebeM unique?
Bébé M is guaranteed 100% organic & plant based (Vegetarian), milk-free and gluten-free. The vision behind their products is built on a unique nutritional, industrial, and ecological approach: 100% vegetable, based on rice protein hydrolyzate, certified organic farming, without milk or gluten, without added sugar or salt, and without soy and palm oil. Bébé M developed delicious formulas adapted to everyone's needs, from infants to young children.
What ingredients make BebeM formulas special?
- Protein intake is provided by an organic rice protein hydrolysate specially developed by Bébé M;
- Balanced fatty acids are provided by coconut, almond, colza, or sunflower oil;
- Slow carbohydrates are provided by naturally gluten-free cereals such as rice, millet, or buckwheat;
- Vitamin D is extracted from Icelandic lichen and not from sheep’s wool;
- Vitamin C is extracted from acerola berries;
- Marine algae provide a mineral contribution.
These are the BebeM formulas we carry:
Bébé M Organic Rice Anti-Reflux (AR) - Stage 1
(age 0 to 6 months)
Bébé M Organic Rice Anti-Reflux (AR) - Stage 2
(age 6 to 10 months)
Bébé M Organic Rice Anti-Reflux (AR) - Stage 3
(age 10+ months)
Please note: This BebeM is labeled "Foods for Special Medical Purposes (FSMPs)" and should only be given under medical supervision. Please consult your pediatrician before introducing the formula to your baby.
Is there a cure for baby eczema?
There is no known cure for baby eczema or eczema in general. Eczema is a chronic condition characterized by inflammation and skin irritation; while it can be managed effectively, it tends to recur periodically throughout life.
The primary goal of treatment for baby eczema is to alleviate symptoms, reduce inflammation, and prevent flare-ups. Treatment typically involves a combination of gentle skincare practices, moisturizers, avoidance of triggers, and, in some cases, medications such as topical corticosteroids or immunomodulators to help control inflammation and itching.
While eczema cannot be cured, many babies with it experience improvement in their symptoms over time, and some may even outgrow the condition as they age.
When to Call a Doctor?

Parents should consider calling a doctor or seeking medical advice if they notice any concerning signs or symptoms of eczema in their baby. If your baby's eczema doesn't show improvement within a week of using over-the-counter hydrocortisone creams, it's advisable to consult your doctor for a prescription medicine.
When seeking medical advice for your baby's eczema, it's essential to ask your doctor relevant questions to understand the condition and its management better. Here are some questions you may consider asking your doctor:
- What is causing my baby's eczema, and how can we determine the triggers?
- What are the best skincare practices and products for managing my baby's eczema?
- Are there any specific dietary considerations or allergens I should be aware of that could be contributing to my baby's eczema?
- What treatments or medications are available for managing my baby's eczema, and what are their potential side effects?
- How often should I apply moisturizers or prescribed medications to my baby's skin, and how long will it take to see improvements?
- Are there any lifestyle changes or environmental adjustments I can make at home to help alleviate my baby's eczema symptoms?
- Should I be concerned about any complications or long-term effects of my baby's eczema, and how can we monitor for them?
- Are there any signs or symptoms I should watch for that may indicate a worsening of my baby's eczema or the development of complications?
- How frequently should I schedule follow-up appointments to monitor my baby's eczema and adjust treatment as needed?
Baby eczema and baby acne are distinct skin conditions with different causes, characteristics, and treatments. While baby eczema is a chronic inflammatory condition requiring ongoing management, baby acne is a temporary condition that typically resolves independently without intervention.
Any Formula-related questions?
Organic Formula Shop offers safe European formulas for peace of mind and comfort. It’s key to know that you are giving your baby nutrition that mimics breast milk as closely as possible and is made with premium organic ingredients. Contact our dedicated customer support team at Organic Formula Shop for expert advice and guidance tailored to your baby's needs. They have earned hundreds of 5-star reviews from our customers, helping you to provide the best nutrition for your little one. Contact us here or shoot us an email at support@organicformulashop.com.
Always Consult Your Pediatrician
This article is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your pediatrician when choosing a formula for your baby. Your pediatrician can help you determine which formula is best for your baby's needs and can provide guidance on introducing a new formula to your baby's diet.